Case of the Fortnight #2
Case of the Fortnight:
By Dr Srinivas BH (PDCC in Renal&Transplant Pathology) Additional Professor. JIPMER. Puducherry
24yr old female case of PCOD and infertility. Presented with vomiting, loss of appetite. H/o of herbal medicine for 2months S. Creatinine 11.3 mg/dl. Anemia: (HB 7.6gr/dl) Urine microscopy: Trace Proteinuria; WBC 5-6/HPF RPRF ?AIN Renal Biopsy performed.
Case of the Fortnight # 2: By Dr Srinivas BH (PDCC in Renal&Transplant Pathology) Additional Professor. JIPMER. Puducherry
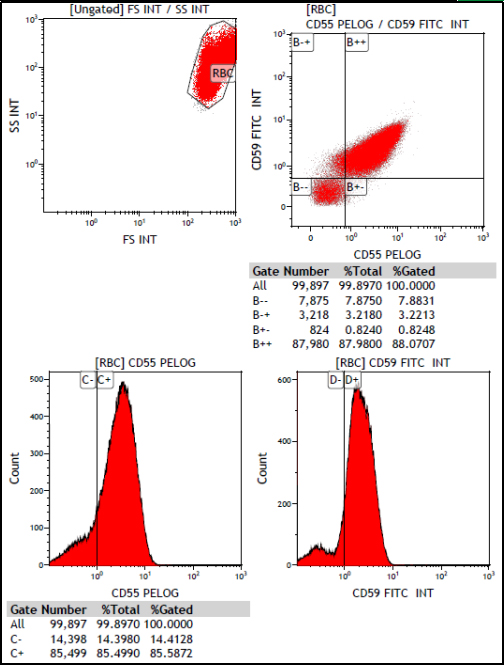
Special thanks to Dr Rakhee Kar Professor for flow cytometry
- 24-year-old lady, case of PCOD and infertility, presented with vomiting and loss of appetite
- H/o of intake of herbal medication for 2months
- S. Creatinine 11.3 mg/dl. Hemoglobin 7.6 gm/dl
- Urine microscopy: Trace Proteinuria; WBC 5-6/HPF. RPRF
- Clinical Diagnosis:?AIN Renal Biopsy was performed.
- 24-year-old lady, case of PCOD and infertility, presented with vomiting and loss of appetite
- H/o of intake of herbal medication for 2months
- S. Creatinine 11.3 mg/dl. Hemoglobin 7.6 gm/dl
- Urine microscopy: Trace Proteinuria; WBC 5-6/HPF. RPRF
- Clinical Diagnosis:?AIN Renal Biopsy was performed.
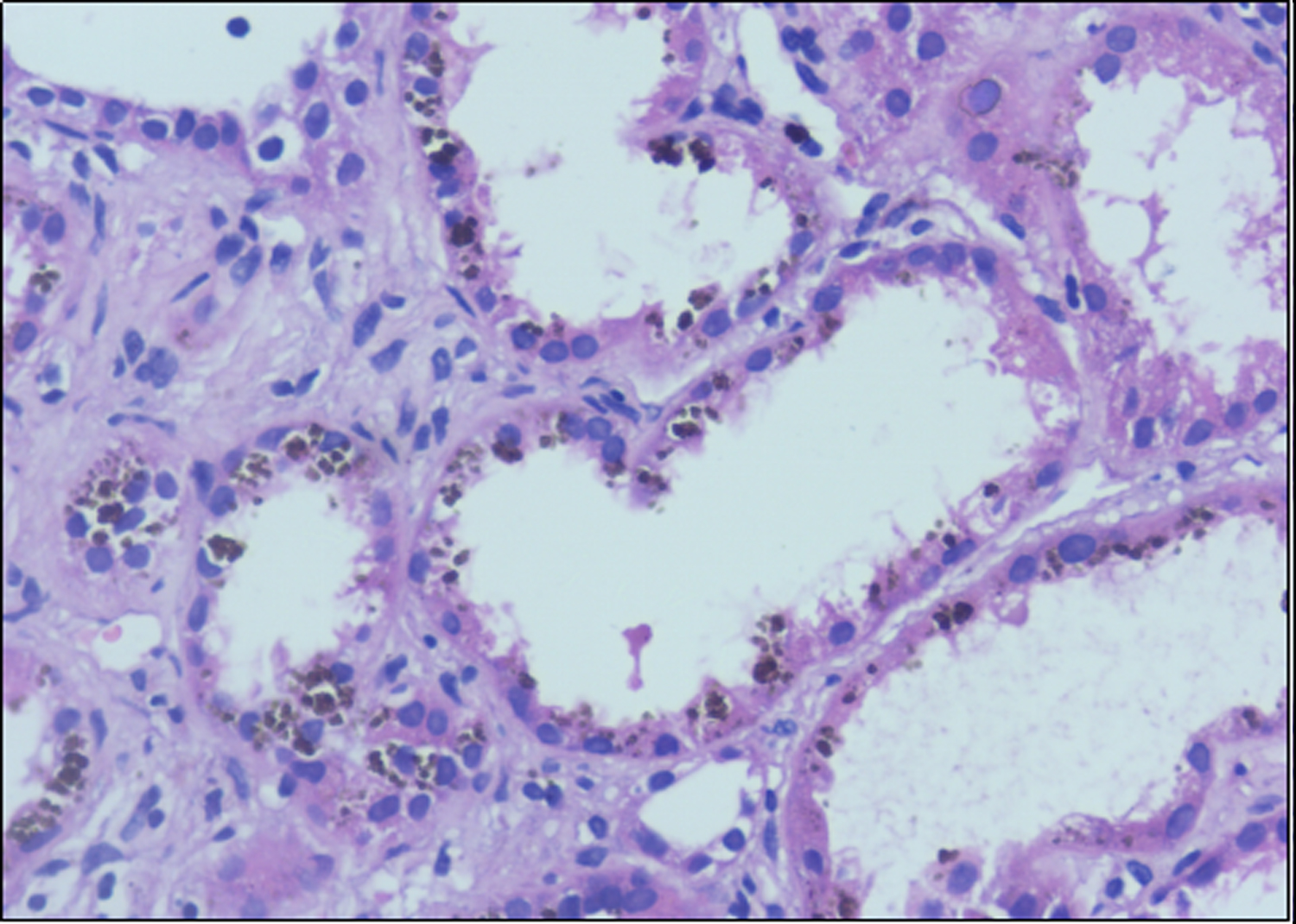
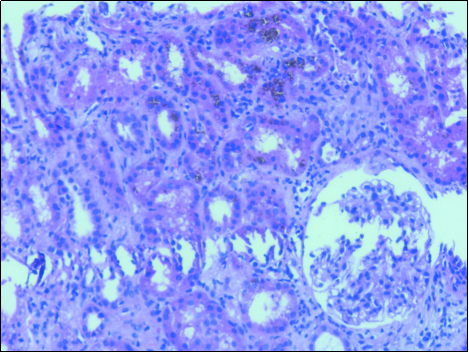
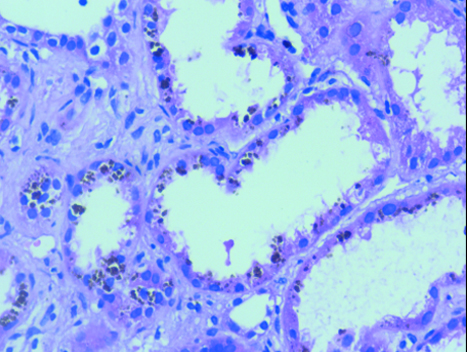
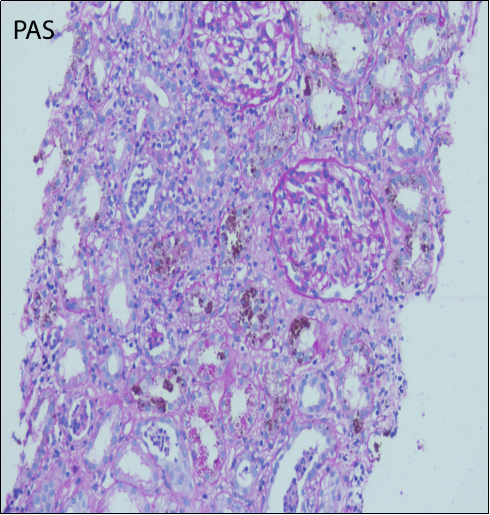
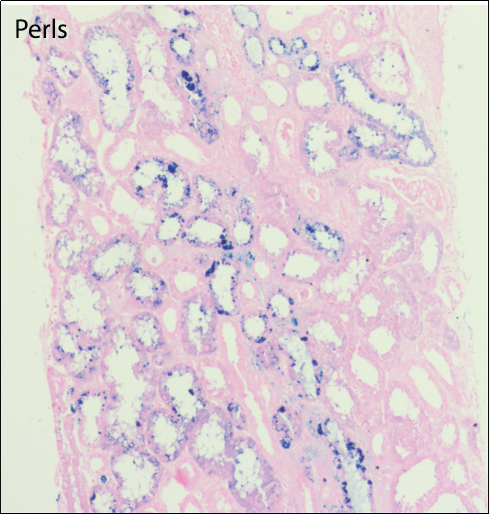
Fig 1&2: H & E-stained sections showing normal glomeruli and prominent intracytoplasmic golden-brown pigment in tubular epithelial cells.
Final Diagnosis
Renal involvement in Paroxysmal nocturnal hemoglobinuria
LEARNING POINTS:
- 1)Paroxysmal nocturnal hemoglobinuria (PNH) is a rare, acquired, potentially life‑threatening disease of blood, characterized by complement‑induced intravascular hemolytic anemia and thrombosis
- 2)Deficiency of the GPI‑anchored complement regulatory proteins such as CD55 and CD59 accounts for the intravascular hemolysis which is the primary clinical manifestation of the disease.
- 3)Renal failure as the primary presentation leading to subsequent diagnosis of PNH is even rarer
- 4)Usually patients present with acute(AKI) on chronic renal insufficiency with increased serum creatinine.
- 5)Renal biopsy shows varied histologic manifestations of acute tubular injury ranging from loss of brush border, cytoplasmic vacuolation, cellular swelling to extensive necrosis of tubular cells, flattening of lining epithelium, cytoplasmic basophilia and prominent golden-brown pigment& red blood cell casts
- 6)Occlusion of the distal tubules by the haemoglobin precipitates causes stasis of urine and allows greater time for endocytosis of hemoglobin from the PCT, and the iron released from its dissociation could cause free radical injury
- 7)Repeated toxic injury to the basement membrane of the tubules leads to punching of holes in the basement membrane and subsequent percolation of the glomerular filtrate into the interstitium, giving rise to inflammation and fibrosis leads to chronic kidney disease (CKD)
- 8)Differential diagnosis: different types of infections like malaria and h/o drug usage
- 9) Treatment with eculizumab , preventing the cascade of events that lead to recurrent and chronic hemolysis, may improve CKD
- 10)Urine sediment shows Prussian blue positive RBC casts
- 11)Flow cytometry is more sensitive in comparison to gel card test and Ham’s and sucrose lysis tests.
- 12)PNH clone size of RBCs is usually less than granulocytes/monocytes due to preferential hemolysis of the PNH clone. Transfused RBCs if any also interfere in RBC clone size. Hence flow cytometric assessment of WBCs gives a better picture.
- 13)PNH can sometimes present directly with renal manifestations, without showing any hematological manifestations. Therefore, its essential for clinicians and pathologists to be aware of the spectrum of renal changes in PNH
REFERENCES:
1)Hill A, DeZern AE, Kinoshita T, et al. Paroxysmal nocturnal hemoglobinuria. Nat Rev Dis Primers. 2017;3:17028. doi: 10.1038/nrdp.2017.28
2) Ram R, Adiraju KP, Gudithi S, et al. Renal manifestations in paroxysmal nocturnal hemoglobinuria. Indian J Nephrol. 2017;27(4):289–293
3) Puri V, Gandhi A, Sharma S. Renal biopsy in paroxysmal nocturnal hemoglobinuria: An insight into the spectrum of morphologic changes.Indian J Nephrol 2017;27:284-8.